Cataract surgery has evolved through many stages. This evolution has included both surgical techniques and devices, which offer patients a combination of optimised post-surgical vision and greater convenience.
Low power cataract surgery, pioneered in Australia by Dr Ilan Sebban, could be the next sign post on the road map to delivering best practice outcomes for patients. This overview describes the low power cataract surgery technique and its key clinical benefits.
WRITER Dr Ilan Sebban
LEARNING OBJECTIVES
-
Understand innovations in cataract surgery and surgical procedures leading to the development of the low power phaco one chop technique
-
Appreciate technical differences between divide and conquer and low power options
-
Identify pre-operative considerations and patient selection for low power cataract surgery
-
Enable broader discussions with patients including pros and cons of surgical options, topical anaesthesia, peribulbar block and consecutive bilateral cataract removal.
—————————————————————————————————–
In 1967, Kelman introduced ultrasonic phacoemulsification for cataract removal.1 This technique has proved to be a safe and effective way to remove the cataract lens.
The introduction of the continuous curvilinear capsulorrhexis by Gimbel and Neuhann in the early 1990s solved many critically important problems for phacoemulsification surgeons.2However, it also created a new challenge – restricted view of the nucleus and then the efficient removal of the 8–10mm nucleus through a 4–6mm capsular opening.
Gimbel proposed the divide and conquer method where the nucleus is fractured within the capsular bag using the phaco tip and surgical spatula.3 This method was further modified by Shepherd when he proposed two deep grooves in the nucleus that intersect centrally, followed by cracking the nucleus into four quadrants.
Kunihiro Nagahara followed in 1993 with an alternative approach that used a horizontal chopping technique. This formed the basis for the phaco chopping techniques specialists use today.
During a phaco chop procedure, the phaco tip is embedded in the nucleus and performs a lamellar dissection of the nucleus as a deep central trough is sculptured. A second instrument is then used, which has a sharp chopper at the end of a needle.
Phaco chopping has evolved into a series of horizontal and vertical chopping techniques, arriving at Paul Kock’s ‘stop and chop’ method.
Essentially the chop methods reduce the high resultant total ultrasound energy that is required to saw through the nucleus. What’s more, the instrument forces are directed centripetally inward and away from the capsular bag and zonules.
The Low Power Cataract Surgery technique is the next manifestation of the phaco chop techniques, where a singular trough through the cataract is used together with viscoelastic to break the cataract up into pieces. This process was published under the name of the Phaco-One Chop Nucleotomy4 by Dr Illan Sebban and has three main phaco phases:
-
Embedding the phaco tip and chopping
-
Flipping the right heminucleus without nucleus rotation, and
-
Evacuating the remaining left heminucleus in the
Ultimately, the divide and conquer and the phaco chopping techniques share one vital characteristic: they lay the foundation for the disassembly of the nucleus into smaller fragments. The main difference between them is the amount of total ultrasonic power delivered into the eye during cataract surgery, measured as Effective Phaco Time (EPT).
WHAT IS THE EXPECTED EPT DATA?
A paper published in 20024 evaluated 198 eyes that had the phaco one chop procedure. Eighty six per cent had a lens opacities classification system III cataract grade of three to six. EPT – a measurement of the total phaco ultrasonic power used during surgery – was 1.9 seconds. For the most dense cataracts, the highest phaco power needed was 5.3 per cent. The mean overall power was 2.1 per cent.
The Alcon Centurion Vision System converts EPT to a total indication of ultrasound power delivered into the eye, called CDE (Cumulative Dissipated Energy). Most times the low power procedures have a final CDE result of under 5 per cent, whereas scores of 5 per cent or higher could result in increased corneal endothelial cell stress, increasing the risk of cellular loss and short and long term corneal oedema. Divide and conquer techniques could potentially result in CDE scores of 5 to 15 per cent or greater.
In summary, the phaco one chop method requires less EPT while offering the surgeon greater control over surgical efficiency and predictability than the techniques it was derived from.
Low Power Surgery: Dr Sebban keeping tight control on the EPT and phaco settings
“the phaco one chop method requires less EPT while offering the surgeon greater control over surgical efficiency and predictability than the techniques it was derived from”
———————————————————————————
SURGICAL ADVANTAGES OF THE LOW POWER TECHNIQUE
There are essentially four advantages of the various phaco-chop methods:
Reduced Phaco Energy and Heat Delivery
The chopping techniques eliminate the need for extensive lens sculpting used in divide and conquer, simply because phaco ultrasound energy is not required to subdivide the nucleus and is only reserved for the phaco assisted aspiration of the fragments.
In the various chopping methods, using a deep central trough allows a marked reduction in EPT. The use of viscoelastic to break apart the cataract, high vacuum rates of up to 650mmHg and aspiration flow rates of up to 45 cc/min, increases the fluid turbulence and allows the fragments to be forced up into the shaft of the phaco tip. This further reduces the EPT, which is particularly important in reducing the risks of corneal endothelial cell stress and eventual loss, as well as wound burn.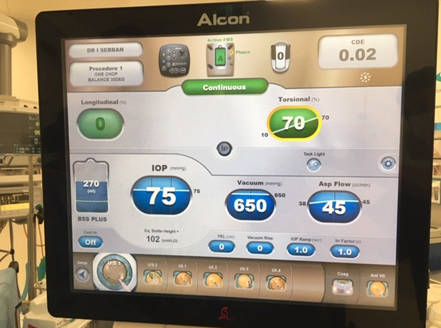
Alcon Centurion Vision System: showing Vacuum Rate of 650mmHg and Aspiration Rate of 45 cc/min.
Reduced Stress on the Zonules and Capsular Bag
With divide and conquer surgery, the capsular bag can immobilise the nucleus during sculpting and a large rigid lens can directly transmit instrument forces, which include those used in sculpting, rotation and cracking, to the capsular bag and zonules.
However, with the various chopping methods, the phaco tip braces and immobilises the nucleus against the instrument’s mechanical forces. What’s more, the forces are directed inwardly, which results in less stress overall on the capsular bag and zonules.
Supracapsular Emulsification
With phaco chop, nuclear fragments are not emulsified until they are removed and elevated out of the capsular bag. This allows virtually all of the phacoemulsification to be performed centrally and within the pupillary plane. As a result, a safe distance is created from both the endothelium and posterior capsule. This procedure also decreases the risks of cutting the iris or the capsulorrhexis edge.
Decreased Reliance on the Red Reflex
Sculpting techniques, such as divide and conquer, rely on visualising the red reflex to judge the depth of the phaco tip and its proximity to the posterior capsule. In contrast, the instrument manoeuvres performed during the chopping methods are more tactile. This is particularly advantageous in the presence of a poor red reflex with diminished corneal clarity, smaller pupils and mature nuclear or cortical cataracts.
ADVANTAGES OF THE PHACO CHOP PROCEDURE
-
Reduced Phaco Energy And Heat Delivery
Ultrasound energy isn’t necessary for the subdivision of the nucleus and is instead used for the phaco assisted aspiration of cataract fragments. -
Reduced Stress on the Zonules and Capsular Bag
The phaco tip that holds and steadies the nucleus in place acts as a buffer against the mechanical chopping force. The manual forces generated by this tip pushing against the other replaces the need for ultrasound energy to cut through the nucleus. -
Supracapsular Emulsification
Nuclear fragments are not emulsified until they’ve been lifted out of the capsular bag. This means nearly all phacoemulsification can be done at a safe distance away from both the endothelium and posterior capsule. -
Decreased Reliance on the Red Reflex
Since it’s not necessary to visualise the exact depth of the phaco tip, chopping is better suited in patients where there is a poor red reflex because of low clarity in the cornea, smaller pupils or even cortical cataracts.
CATARACT SURGERY AND CORNEAL ENDOTHELIAL CELL LOSS
The role of the corneal endothelium is to maintain the correct level of corneal hydration. It forms a physical barrier between the corneal stroma and aqueous humour and acts as an ion pump.
A normal corneal endothelium is a single layer of uniformly sized cells with a predominantly hexagonal shape. Adult density is in the range of 2,400–3,200 cells/ mm². The number of cells decreases at about 0.6 per cent per year and neighbouring cells enlarge to fill the space as the endothelial cells cannot regenerate. The minimum cell density necessary for adequate function is in the range of 400–700 cells/mm2.
The effect of cataract surgery on corneal endothelium is an important factor that affects postoperative vision. It is accepted that there is definite loss of some endothelial cells with all cataract surgery techniques. In the past, cataract surgery caused an enormous loss of endothelial cells. With today’s enhanced equipment and surgical techniques, modern cataract surgery is much less damaging, resulting in 6–14 per cent loss of endothelial cells.
In normal circumstances, the reserves of endothelial cells mean there are enough to last a lifetime. However, if a significant number of cells are injured, this causes a significant decrease in endothelial cell density, which can impair the endothelium’s ability to maintain corneal clarity. This results in irreversible corneal edema, where the patient will experience permanent blurring in their vision as well as ocular pain.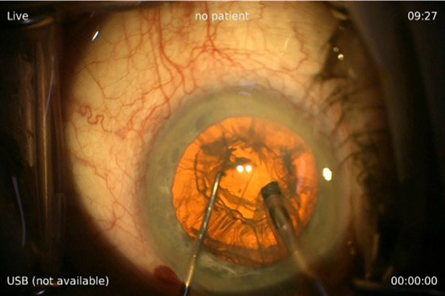
Low Power Cataract Surgery: Holding the phaco tip with the right hand and chopper with the left hand
“Using a phaco one chop nucleotomy procedure reduces the EPT to a matter of seconds with the total surgical time possibly reduced down to approximately 6 to 10 minutes per eye”
———————————————————-
Excessive duration of phacoemulsification may result in increased corneal endothelial cell stress, resulting in stromal striata with or without oedema.
The ultrasound energy used in phacoemulsification is also associated with the production of free radicals. Free radicals are reactive species with one or more unpaired electrons in their outer orbits. Such chemicals can cause damage to the corneal endothelium known as oxidative stress.
In the extreme, pseudophakic bullous keratopathy describes the irreversible oedema and endothelial cell damage that occurs after cataract surgery. The advent of phacoemulsification techniques and the use of intraocular lenses (IOLs) and ophthalmic viscosurgical devices have helped to reduce the number of cases of pseudophakic bullous keratopathy following cataract surgery.
However, it is important to note that the most common cause of corneal endothelial decompensation is still surgical trauma. Corneal endothelial cell loss (ECL) is increasingly a clinical consideration for surgeons and their patients. The sustained and prolonged use of phaco ultrasound during cataract procedures has been found to damage the cornea resulting in swelling. At best, patients experience blurred vision for a few weeks or even months post surgery. However, the risk of long lasting, or even permanent corneal oedema could be higher with the divide and conquer methods.
BENEFITS OF PHACO CHOP TECHNIQUE
-
Reduced EPT
-
Reduced capsular and zonular stress
-
Decreased red reflex reliance
-
Supracapsular and central location of emulsification
———————————————————————-
CATARACT AND CORNEAL DISEASE
Decreasing the EPT delivered into the eye during cataract surgery is particularly important in patients with compromised corneas. These include Fuch’s dystrophy, previous corneal transplantation and refractive surgery, as well in patients with dry eye and psuedoexfoliation.
Fuch’s dystrophy can affect up to 4 per cent of the adult population. These patients present with endothelial cell loss and guttata on the Descemet’s membrane. Patients with cataracts can present a particular challenge with the divide and conquer method as surgeons are faced with the dilemma of whether or not they should recommend cataract removal.
Reducing the ECL loss could also reduce the risk of requiring an endokeroplasty – descemet stripping automated endothelial keratoplasty or descemet’s membrane endothelial keratoplasty – either during or post surgery.
Reflections on surgical experience
Reducing endothelial cell stress and loss (ECL) is a major consideration in cataract surgery today and I believe it’s a good reason to offer phaco one chop and low power surgery options.
When performing cataract surgery, I prefer to use high vacuum rates of up to 650mmHg and aspiration flow rates of up to 45 cc/min. I know that some surgeons don’t like to use high flow rates because it may cause ECL when a lot of fluid passes by the cornea, but on balance, if anything is causing ECL it is the total energy delivered into the eye. My surgeries are quick, only requiring topical anaesthetic. By contrast, divide and conquer procedures are generally longer, so even if there is low flow, the final EPT may be higher because of the longer surgical time.
If a patient experiences reduced vision post surgically it may be that the corneal endothelium has experienced stress or ECL.
CONSEQUENCES OF HIGH POWER
In my experience, I aim to use lower than 5 per cent CDE, as indicated on the Alcon Centurion Vision System. If the surgery results in a CDE of 5 per cent or higher, there is most likely increased ECL stress. Occasionally the divide and conquer can deliver a CDE up to 15 per cent or even up to 30 per cent. Even though the short term corneal odema may be mild and self correcting, the patient still experienced mild swelling in the cornea.
“I feel low power cataract surgery offers the best possible results for my patients’ vision in both the short and long term”
We’re simply trying to keep the delivered power during surgery as low as possible, the study conducted in 20024 demonstrated that phaco chopping with high vacuum and high flow actually reduces the EPT and therefore reduces the risk of corneal edema or endothelial cell loss.
PREOPERATIVE COUNSELLING
As new technologies emerge alongside the refinement of surgical techniques, we are entering an era where all patients can benefit from excellent and often spectacle free vision following cataract surgery. Clearly, the days of ‘one size fits all’ have ended – that’s why it’s vital that surgeons establish a strong relationship with patients.
The initial consultation is just as – if not more – important than the scheduled cataract surgery. It is vitally important to use this consultation to get to know the patient with discussion that extends beyond the cataract surgery itself. Does the patient have children? Is the patient still working? What are their hobbies? You’ve got to work out who they are, understand their lifestyle demands and their expectations prior to surgery. This is paramount to successful outcomes – you almost need to be a novice psychologist!
IOL SELECTION
Selecting intraocular lenses for patients must also be based on these discussions.
Contrary to popular belief, the use of multifocal lenses in cataract patients, while common, isn’t necessarily a foregone conclusion. Some patients genuinely don’t like these lenses because they can produce halos and rings and no one’s happy. I counsel all my patients on multifocal lenses before surgery so they can make informed decisions.
Today’s IOL designs offer a variety of lenses including Extended Depth of Focus lenses (EDoF), which, as a lens, is actually very benign – although it’s not a standard monofocal lens it allows almost every patient to benefit by having a bit more depth in their intermediate vision post surgery. This also gives patients the post surgical freedom to participate in hobbies, see their food, their speedometer while driving, and their phones and computer comfortably, while still maintaining high levels of binocularity in an unaided environment. EDoF lenses are very safe to use for patients who have glaucoma or epithelial membranes, even with visual field loss, and can be easily tolerated.
PATIENT FEEDBACK
Over a long medical career I have been fortunate to improve the vision of patients from every walk of life. Their consistently good feedback is a great source of professional satisfaction.
I have drawers full of letters from satisfied people. I’ve operated on sculptors and painters so I’ve got a house full of art! I want to give my patients – whatever their age – clear and comfortable vision, not just distance or mono vision. My mission statement is to give them binocularity at all distances.
I believe that as a surgeon, you should always strive to be affable and present the patients with perceived value for money surgical options – the reality is that referrals can be influenced by the patient’s ‘out of pocket’ expenses.
Having sailed both Sydney to Hobart and across the Trans-Tasman ditch – an eight day journey each way – I have encountered some massive seas. Most recently, I experienced 60 knot winds with 5–10 metre waves and had to sail 48 hours without sleep. I didn’t have any fear as I had done my due diligence and knew we were on course although it was challenging! Similarly, our role as eye care professionals is to work diligently to provide best practice outcomes. That’s why I feel low power cataract surgery offers the best possible results for my patients’ vision in both the short and long term.
TOPICAL ANAESTHETIC AND THE LOW POWER TECHNIQUE
Using a phaco one chop nucleotomy procedure reduces the EPT to a matter of seconds with the total surgical time possibly reduced down to approximately 6 to10 minutes per eye. This allows the option of using topical anaesthesia, which can be combined with low level sedation.
There are several benefits to using topical anaesthesia both for the surgeon and the patient, that include increased theatre efficiency and reduced costs. Topical anaesthesia is especially beneficial for the 60+ population bracket – the most common age demographic of cataract patients. In cataract surgery, it is arguably the safest anaesthetic method, and can be carried out with a number of different agents including 2 or 4 per cent Lignocaine or 1 per cent Naroprin (Ropivocaine).
One per cent Naroprin is often the drug of choice as it can be longer lasting, less toxic to the epithelium and well tolerated by the patient with less initial stinging sensation upon instillation.
The combination of drugs used for gastroscopy/colonoscopy procedures can generally be used for low level sedation when performing the low power technique, ie. Midazolam 0.5–2mg, Propofol 5–10mg and Fentanyl 12.5 to 25ug.
What’s more, the faster surgical time infers that the peri-bulbar block injection may not be necessary. Retrobulbar and peribulbar anaesthesia carry real risk of morbidity, and the incidence of persistent
diplopia could be as high as 0.25 per cent. Other complications include ipsilateral globe penetration, transient contralateral amaurosis, respiratory arrest, and anterior ischemic optic neuropathy secondary to retrobulbar hematoma.
Combining topical anaesthesia without any retrobulbar block allows the patient to see clearly immediately after surgery. The operated eye does not need patching and is only covered with a clear protective patch post surgically. Even though this ability to see clearly straight after surgery has only a one day benefit over traditional surgery, it is particularly appreciated by monocular patients.
Another positive outcome of using topical anaesthesia is that patients can be offered the option of bilateral cataract surgery on consecutive days. This removes the discomfort of the resulting anisometropia caused by the delay between surgeries, which can extend to weeks or months in some cases.
BENEFITS OF LOW POWER CATARACT SURGERY
-
Local anaesthetic
-
No peribulbar block
-
Quicker recovery time
-
Bilateral surgery on consecutive days
-
Cost effective for patients
-
Ease of follow-up care

Local anaesthetic: Requires close observations and co-ordination of the surgeon, scrub nurses and anaesthetist.
DRIVE THE PHACO EMULSIFICATION MACHINE LIKE A FERRARI
One of the key pieces of equipment used in cataract surgery, whether it’s divide and conquer or the phaco one chop, is the phacoemulsification device, yet this powerful system is commonly under used.
Highly engineered systems like Alcon’s Centurion Vision System have potential to allow high vacuum and aspiration settings to be used safely and efficiently – a fitting analogy could be ‘it’s like having a Ferrari but driving it like a Toyota’. This sports car reference may attract attention and inspire a laugh or two, however the benefits of using the full potential of your phacoemulsification device or ‘driving it like a Ferrari’, can offer significantly enhanced surgical outcomes.
To earn your CPD points from this article answer the assessment available at mivision.com.au/low- power-cataract-surgery
 mivision • ISSUE 141 • FEB 19
mivision • ISSUE 141 • FEB 19
mieducation
References
-
Hassan G, ‘Divide and conquer versus chopping in phaco-emulsification’ Menoufia Medical Journal 2016, 29:627-631
-
Colvard Michael D, ‘Achieving Excellence in Cataract Surgery’ 2009, 5:33-41
-
Gimbel HV, Neuhann ‘Development, advantages and methods of the continuous curvilinear capsulorrhexis’, Journal of Cataract and Refractive Surgery 1991: 17: 110-111
-
Sebban I, ‘One Chop Nucleotomy’, Journal of Cataract and Refractive Surgery 2002, Aug 28(8): 1325-1329






 Book online
Book online